You get a lot more from a day at the beach than just fresh air. For one, you get vitamin D! This essential nutrient, which is integrally involved in many vital bodily processes, is derived both from sun exposure, and to a far lesser degree, from the food we eat.
But even if you live in a sunny climate, it's entirely possible that you're not getting nearly as much as you should. If so, you're probably in the majority, since the Centers for Disease Control and Prevention have estimated that over half the population of the United States is deficient in vitamin D.[1]
That's something to take note of even in so-called "normal" times, but especially during the COVID-19 crisis, when some new studies are finding that patients with severe cases often also have low vitamin D levels.[2] This doesn't mean that Vitamin D will protect you from the virus, but it shows how important this nutrient is to keeping your body strong and resilient overall.
Especially since so many people are indoors—i.e., out of direct sunlight—these days, it's normal if you're wondering: Is vitamin D supplementation right for me? Read on!
What Is Vitamin D?
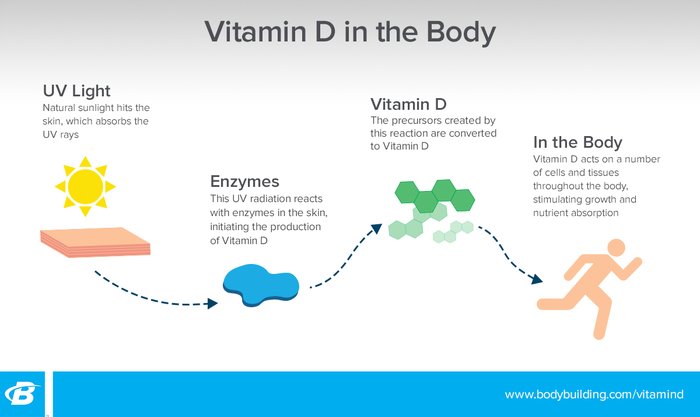
Vitamin D is known as the sunshine vitamin, but it's not technically a vitamin. It's actually considered a pro-hormone, and it is synthesized though the skin in a reaction to sun exposure. Once created, vitamin D acts on a number of cells and tissues throughout the body to stimulate growth and absorption of nutrients.
There are two common forms of this vitamin, D-2 and D-3, which are very different in both structure and function.[2] D-2 is synthesized through plant irradiation and has much less bioavailability than its counterpart. D-2 is not made by the human body, and has one-third of the uptake that D-3 has, making it much less beneficial for humans.[3]
D-3, on the other hand, is made both by the body and when taken exogenously, and is highly bioavailable. For this article's sake, when vitamin D is discussed it is in reference to the more bioactive D-3.
What Does Vitamin D Do?
Vitamin D is used by the brain, skeletal muscle, colon, bone, heart, adrenal glands, and even immune cells. It helps regulate mineral absorption, mood, and insulin sensitivity, among other processes.
It's estimated that almost 50 percent of people worldwide have a vitamin D deficiency, or at minimum, a vitamin D insufficiency.[4] Even though most of us have access to the sun's powerful rays, vitamin D deficiency is common when skin is shielded from the sun, or in those with darker skin pigments.[5]
What Are the Dangers of Vitamin D Deficiency?
Stress Fractures: The role of Vitamin D in calcium and phosphorous absorption makes a deficiency in this nutrient a threat to bone integrity. It could be especially dangerous for those already prone to stress fractures and osteoporosis, such as distance runners, female athletes, and the elderly.

Depression: D deficiency could also cause you to feel sluggish, depressed, and maybe even "SAD". According to the American Academy of Family Physicians, 10-20 percent of Americans may have a mild depressive disorder called Seasonal Affective Disorder (SAD).[6] This feeling of overall fatigue, heaviness, and insomnia, accompanied with weight gain, is most commonly diagnosed in the winter months.
It's estimated that 1 in 7 people suffer from symptoms of depression at some point in their life, whether from SAD or other causes.[7] Some of these depressive symptoms can be caused by neurotransmitter or hormone imbalances. Vitamin D creates a favorable environment for the production of feel-good hormones and may help support a healthy mood.
Impaired Muscle Recovery: Studies have also touted vitamin D's effect on skeletal muscle. A study out of Liverpool John Moores University found that six weeks of supplementation with 4,000 IU a day of vitamin D improved muscle recovery in the days after a tough workout.[8] If you train hard, especially if you're prone to sprains and tears, it's definitely worth considering taking supplemental vitamin D to help maximize your recovery and lower your chance of injury.
It's worth noting that while not getting enough vitamin D can lead to these conditions, supplementing won't bulletproof you. It can reduce your risk, but not eliminate it. And getting more than enough won't give you any additional performance benefits above the normal range. In other words, once you've erased your deficiency, any extra vitamin D won't continue to help you in your quest to become Wolverine.
How Much Vitamin D Do You Need?
The recommended daily allowance for vitamin D is 400-800 IU per day, but as Jonny Bowden writes in the article "D Up: The Case for More Vitamin D," many adults could likely benefit from more—even if they spend ample time in the sun. Conservatively, 5,000 IU is a safe daily dose for adults and 1,000 IU per 25 pounds of body weight is considered safe for children.[9]

Are There Any Side Effects? What Happens If You Take Too Much?
The upper limit of safe vitamin D supplementation is thought to be around 10,000 IU per day, and it's much more common to be deficient than overdosing.[11] Still, watch out for warning signs if you take vitamin D supplements. Side effects of vitamin D toxicity include weakness, lethargy, headaches, and nausea. If you think you might be deficient in vitamin D and are considering supplementation, or if you think you might be taking too much, talk to your doctor.
What Are the Possible Interactions With Medications?
Vitamin D is considered a safe supplement with most medications, but always check with your physician before starting any new supplement regimen. Vitamin D is fat-soluble, so interactions could occur from supplements that block fat absorption or from a very-low-fat diet. Corticosteroids are also known to decrease the absorption of vitamin D by lowering calcium absorption.[4]
Are There Any Dietary Forms of Vitamin D?
The main way humans get vitamin D is from the sun.
According to the Vitamin D Council, there are very small amounts of vitamin D naturally available in foods, and it is not likely to meet sufficient needs through foods alone.[10] These foods include egg yolks, fatty fish, beef liver, fortified milk, and orange juice. Unfortunately, many companies claim to fortify foods with vitamin D but are simply incorporating D-2, the nearly non-bioavailable form of vitamin D.[3] So don't believe every label you read!

What Are the Available Forms of Vitamin D Supplements?
Vitamin D can be taken though several different forms, including drops taken orally, and tablets or capsules. According to a 2014 study, drops, powdered capsules, and chewable supplements are all similarly effective, provided they contain the D-3 version of the vitamin.[12]
How and When Should You Take Vitamin D?
Because it is fat-soluble, vitamin D is best taken with a fat source or a meal. And even if you take a supplement, getting outside and being active is a great way to increase vitamin D levels in the blood naturally. However, if you live at latitudes above 35 degrees (which is most of the U.S.), or have dark skin, it's possible you'll synthesize less vitamin D through the skin, at which point oral supplementation is a good idea.
If you're getting your vitamin D from the sun, the best time for increasing synthesis is midday, when your shadow is shorter than you. While it makes sense to go without sunscreen when vitamin D is the goal, normal sunscreen usage may not negatively affect the amount of vitamin D you synthesize, according to British and Australian studies.[13,14] But if you don't wear sunscreen, you're at greater risk of getting sunburned! In that case, stay in the sun for half the time it takes your skin to turn pink. Too much sun can destroy vitamin D in the skin, so this isn't a license to lay out slathered in baby oil all afternoon.
Vitamin D is a powerful nutrient, and a lot of us would benefit from getting more of it. Don't count on your diet to give it to you! Get out in the sun, and if you have doubt about that being enough, consider optimizing your intake with a supplement.
References
- Looker, A. C., Johnson, C. L., Lacher, D. A., Pfeiffer, C. M., Schleicher, R. L., & Sempos, C. T. (2011). Vitamin D status: United states, 2001–2006. NCHS Data Brief, 59(59), 1-8.
- Daneshkhah, A., Agrawal, V., Eshein, A., Subramanian, H., Roy, H. K., & Backman, V. (2020). The Possible Role of Vitamin D in Suppressing Cytokine Storm and Associated Mortality in COVID-19 Patients. medRxiv
- Norman, A. W. (2008). From vitamin D to hormone D: fundamentals of the vitamin D endocrine system essential for good health. The American Journal of Clinical Nutrition, 88(2), 491S-499S.
- Armas, L. A., Hollis, B. W., & Heaney, R. P. (2004). Vitamin D2 is much less effective than vitamin D3 in humans. The Journal of Clinical Endocrinology & Metabolism, 89(11), 5387-5391.
- Nair, R., & Maseeh, A. (2012). Vitamin D: The "sunshine" vitamin. Journal of Pharmacology & Pharmacotherapeutics, 3(2), 118.
- Holick, M. F. (2007). Vitamin D deficiency. The New England Journal of Medicine, 2007(357), 266-281.
- Teegarden, D., & Donkin, S. S. (2009). Vitamin D: emerging new roles in insulin sensitivity. Nutrition Research Reviews, 22(1), 82-92.
- Seasonal Affective Disorder. (2000, March 01). Retrieved September 18, 2017, from http://www.aafp.org/afp/2000/0301/p1531.html
- Popa, T. A., & Ladea, M. (2012). Nutrition and depression at the forefront of progress. Journal of Medicine and Life, 5(4), 414.
- Owens, D. J., Sharples, A. P., Polydorou, I., Alwan, N., Donovan, T., Tang, J., ... & Close, G. L. (2015). A systems-based investigation into vitamin D and skeletal muscle repair, regeneration, and hypertrophy. American Journal of Physiology-Endocrinology and Metabolism, 309(12), E1019-E1031.
- Sources of Vitamin D 2017. (n.d.). Retrieved September 18, 2017, from https://www.vitamindcouncil.org/
- Vieth, R. (2007). Vitamin D toxicity, policy, and science. Journal of Bone and Mineral Research, 22(S2).
- Traub, M. L., Finnell, J. S., Bhandiwad, A., Oberg, E., Suhaila, L., & Bradley, R. (2014). Impact of vitamin D3 dietary supplement matrix on clinical response. The Journal of Clinical Endocrinology & Metabolism, 99(8), 2720-2728.
- Norval, M., & Wulf, H. C. (2009). Does chronic sunscreen use reduce vitamin D production to insufficient levels? British Journal of Dermatology, 161(4), 732-736.
- Marks, R., Foley, P. A., Jolley, D., Knight, K. R., Harrison, J., & Thompson, S. C. (1995). The effect of regular sunscreen use on vitamin D levels in an Australian population: results of a randomized controlled trial. Archives of Dermatology, 131(4), 415-421

